In the ever-evolving landscape of health and wellness, the term “biometrics” has been popping up more and more. In fact, wearable technology is projected to be the leading fitness trend in 2024 according to the American College of Sports Medicine (ACSM)!
These devices, often in the form of fitness watches, chest straps, or even rings, capture valuable data points that shed light on an individual’s health and function. From maximum heart rate, total activity levels to sleep quality, these metrics have been extensively utilised in fitness and sports and in recent years, have made their way into the health and rehab space.
Given their relevance and our appreciation of them – we thought it was about time for a deep dive! So read on to learn about our favourite biometric data-point, how we (and research!) believes they can be of use to improve health and function and how you can get started today.
Heart Rate Variability (HRV)
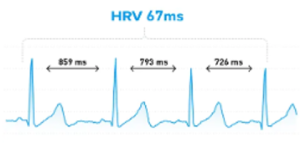
Among these data points, our favourite one, and therefore the one we focus on most, is Heart Rate Variability (HRV). This metric, measuring the variation in time between heartbeats, has garnered significant attention in research. Why? Because HRV serves as a powerful indicator of the autonomic nervous system’s (ANS) function (1,2), which plays a key role in various illnesses (3,4).
To understand HRV, a quick dive into physiology is necessary. The ANS comprises two branches—sympathetic and parasympathetic—responsible for the body’s fight or flight response and rest and digest activities, respectively. A well-functioning nervous system maintains a delicate balance between these two branches.
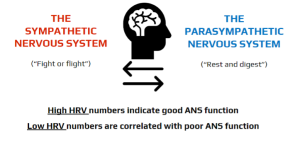
Research tells us that measuring HRV, provides us with an accurate indicator of this balance – AKA by looking at HRV data, we can see how well the nervous system is functioning! Not only this, but by gathering consistent HRV data, we know whether someone has either parasympathetic or sympathetic dominance – AKA are they swinging heavily toward or getting “stuck” in one or the other? (1,2)
Biometrics in the World of “Invisible Illness”
Given the above information, it is no surprise that biometrics can be a useful tool in addressing various health conditions. As exercise physiologists, we use them in a range of contexts, but one context we see their impact the most is the space of “invisible illness.”
This term encompasses conditions or disorders with largely invisible symptoms, such as chronic fatigue, long-COVID, mental health conditions and POTS. These conditions pose unique challenges due to their internal nature and complex symptoms. Biometrics, by offering objective information and a tangible tool, can help to tackle the subjectivity of symptoms, variable and fluctuating symptoms and the lack of individualised rehabilitation programs.
In practice (albeit simplified), a program utilising HRV looks like this:

Perhaps the most crucial factor is the way that biometrics empower conversations that allow us and our clients to gain more insights into their body and symptoms. Some examples of biometrics in use and the conversations they invoke might include:
- Activity data to look at overall movement levels and trends;
“It looks like you did a lot more activity than usual on Tuesday and were forced to rest for 2-days after? We call that booming and busting, let’s look at levelling out your activity in coming weeks – you might even find that you can do more if we can get it more consistent”
- Sleep quality and quantity to assess its impact on symptoms;
“Your sleep scores have really improved over the last 2-weeks, do you think it could be to do with the mindfulness we’ve implemented after work?”
- Heart rate to see how the cardiovascular system is functioning;
“You say you feel exhausted after small tasks like the dishes, but looking at your heart rate of 162bpm, these tasks aren’t small for your body at the moment. We can look to improve this in coming weeks”
- HRV to see how the body is handling all of the above, as well as other more invisible stressors;
“That presentation at work definitely took a toll on the body, but that’s OK, lets include some parasympathetic recovery today”
Yes, that’s right! Not only is HRV sensitive to physical load, HRV is also sensitive to, and therefore provides us with information on non-physical loads (the reason it’s our favourite biometric data-point). Research shows that HRV responds to psychological stress, cognitive fatigue, anxiety and even negative social interactions/experiences, so we can build all of this into the “load” as you would with any physical activity program (5,6,7,8).
Imagine you are someone who has been battling with the frustrations of invisible illness. The ups and downs, the reliance on constantly “checking-in” with your own symptoms, trying to identify and remember patterns. . . biometrics provide relief, validation and a sense of control. They can take away some of the “invisible” in invisible illness, providing a path forward.
Where to start?
Speaking of the path forward, getting started with using biometrics, specifically Heart Rate Variability (HRV) might feel a bit overwhelming. But don’t worry! Here’s a straightforward step-by-step guide to kick off your journey. All you need is a Polar H10 strap, your smartphone, and 90 seconds of quiet time each morning.
- App Setup: Download the “Elite HRV” app on your smartphone.
- Connect Your Device: Sync your Polar H10 heart rate strap with the app.
- Daily Check-In: Follow these steps for your daily HRV check:
- Find a calm spot within 10 minutes of waking up, keeping it consistent each day
- Open the “Elite HRV” app
- Select “Morning Readiness”
- Opt for the 90-second reading while sitting
- Start the reading and sit quietly, following any on-screen instructions
A quick tip: It’s a good idea to gather 2 weeks of data before diving into any deeper analysis.
The app itself will provide you with some great info based on your readings. However, alongside your daily HRV checks, keep a simple diary of your daily activities. After two weeks of data look for patterns. Are there trends or noticeable ups and downs? Do you tend to swing toward a sympathetic or parasympathetic dominance? Do your poorer readings correlate with certain activities/loads? Also, as you try out other strategies to improve your health, like changing your diet, meditating, or exercising, keep an eye on your HRV for extra feedback on whether they are having an impact.
Over time, we are basically aiming for two things:
- More “balanced” readings: Strive for HRV readings that don’t swing wildly from day to day.
- Gradual Score Increase: Look for a slow increase in your average HRV score
These simple signs tell you that you’re on the right track to improved nervous system function. So, enjoy the process, watch for patterns, and let us know how you get on!
Author: Tessa Nielsen
Clinical Exercise Physiologist and
Content Creator at Specialised Health
References:
- Marques, K. C., Silva, C. M., Da Silva Trindade, S., De Souza Santos, M. C., Rocha, R. B., Da Costa Vasconcelos, P. F., Quaresma, J. a. S., & Falcão, L. M. (2022). Reduction of Cardiac Autonomic Modulation and Increased Sympathetic Activity by Heart Rate Variability in Patients With Long COVID. Frontiers in Cardiovascular Medicine, 9. https://doi.org/10.3389/fcvm.2022.862001
- Shih, C., Chou, P., Chen, J., Chou, T., Lai, J., Lu, C., & Huang, T. (2023). Cancer-related fatigue classification based on heart rate variability signals from wearables. Family Medicine and Primary Care, 10.
- Zalewski, P., Słomko, J., & Zawadka‐Kunikowska, M. (n.d.). Autonomic dysfunction and chronic disease. British Medical Bulletin, 128(1), 61–74. https://doi.org/10.1093/bmb/ldy036
- Słomko, J., Estévez‐López, F., Kujawski, S., Zawadka‐Kunikowska, M., Tafil-Klawe, M., Klawe, J. J., Morten, K., Szrajda, J., Murovska, M., Newton, J. L., & Zalewski, P. (2020). Autonomic Phenotypes in Chronic Fatigue Syndrome (CFS) Are Associated with Illness Severity: A Cluster Analysis. Journal of Clinical Medicine, 9(8), 2531. https://doi.org/10.3390/jcm9082531Escorihuela, R. M., Capdevila, L., Castro, J. R.,
- Zaragozá, M. C., Maurel, S., Alegre, J., & Castro-Marrero, J. (2020). Reduced heart rate variability predicts fatigue severity in individuals with chronic fatigue syndrome/myalgic encephalomyelitis. Journal of Translational Medicine, 18(1). https://doi.org/10.1186/s12967-019-02184-z
- Kim, Hye-Geum, et al. “Stress and heart rate variability: a meta-analysis and review of the literature.” Psychiatry investigation 15.3 (2018): 235.
- Hjortskov, Nis, et al. “The effect of mental stress on heart rate variability and blood pressure during computer work.” European journal of applied physiology 92.1 (2004): 84-89.
- Lischke, A., Jacksteit, R., Mau-Moeller, A., Pahnke, R., Hamm, A. O., & Weippert, M. (2018). Heart rate variability is associated with psychosocial stress in distinct social domains. Journal of Psychosomatic Research, 106, 56–61. https://doi.org/10.1016/j.jpsychores.2018.01.005
#exercisephysiology #exerciserehab #rehabilitation #lifeinsurance #incomeprotection #ctp #workcover #mobile #mobileexercisephysiology #fatigue #mentalhealth #cancer #musculoskeletal #injury #pain #physio #physiotherapy #Sydney #Brisbane #Melbourne #Adelaide #Auckland #Waikato #BayofPlenty #Wellington #Otago #Christchurch
