Osteoarthritis, osteopenia, osteoporosis… do you know the difference? These terms may initially seem interchangeable, but their nuances are important.
As Exercise Physiologists, we come across a range of “osteo” conditions, each of which has a different set of implications. In this blog, we’ll dive into the distinct characteristics of two common “Osteo” conditions: osteoarthritis and osteoporosis. That way, you’ll be well-informed when you see or hear them mentioned – whether it’s in relation to your own health, or someone else’s.
Osteoarthritis: A Joint and Cartilage Challenge
Osteoarthritis (OA), often referred to as degenerative arthritis or wear-and-tear arthritis, is the most prevalent form of arthritis, with over 100 types in existence! Doctors may use various terms to describe OA, such as joint deterioration, joint degeneration, bone-on-bone, calcium deposits, bone spurs, and more. If you’ve ever had these discussions, you know how confusing they can be – put simply, OA refers to conditions affecting the joints and cartilage.
In OA, the articular cartilage covering the bone ends adjacent to each other degenerates over time. This degeneration can lead to “bone-on-bone” contact, resulting in pain, inflammation and discomfort.
One key distinction between OA and other forms of arthritis like rheumatoid arthritis is the level of inflammation. OA is characterised by limited inflammation, and any joint swelling is typically temporary and linked to overuse or exertion. Blood tests for inflammation usually yield negative results since inflammation is localised within the joint.
While there’s no medication that can halt OA progression, several treatments are available to manage symptoms. These may include anti-inflammatory drugs, analgesics, and, in some cases, supplements. However, rehabilitation and strength-building exercises are essential components of OA management. Movement overall is crucial for joint health and strengthening the muscles surrounding a joint can help reduce stress and enhance mobility.
Osteoporosis: A Bone Health Challenge
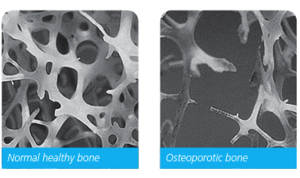
Osteoporosis, often confused with osteoarthritis due to their co-occurrence, is fundamentally a bone health issue. Unlike OA, osteoporosis is typically painless until a fracture occurs. It involves the loss of bone mass, increasing the risk of fractures, especially in the spine, hips, and wrists. So if you receive a diagnosis of osteoporosis, it is important that you are aware of this increased risk.
Osteoporosis commonly starts with low bone mass around age 50, with women often experiencing it after menopause. The condition progresses silently, with bone mass gradually decreasing. Osteopenia, a precursor to osteoporosis, can lead to the condition if left untreated.
Effective osteoporosis management encompasses three key aspects: adequate calcium and vitamin D intake, exercise to strengthen bones and decrease falls risk, and medication when osteoporosis is diagnosed.
Knowledge is Power
This is especially when it comes to conditions like osteoarthritis and osteoporosis. Understanding these conditions not only empowers you to take charge of your health but also guides you towards effective management.
Don’t let osteoarthritis or osteoporosis keep you on the sidelines. With the right approach, you can continue to lead an active and fulfilling life.
Author: Tessa Nielsen
Clinical Exercise Physiologist and
Content Creator at Specialised Health
#exercisephysiology #exerciserehab #rehabilitation #lifeinsurance #incomeprotection #ctp #workcover #mobile #mobileexercisephysiology #fatigue #mentalhealth #cancer #musculoskeletal #injury #pain #physio #physiotherapy #Sydney #Brisbane #Melbourne #Adelaide #Auckland #Waikato #BayofPlenty #Wellington #Otago #Christchurch



