We as a nation and as RTW professionals, have the potential to be leading the powerful trend supporting General Practitioners in taking the initiative to get patients back to work.
Ten years ago The Royal Australasian College of Physicians first released the Australian and New Zealand Consensus Statement on the Health Benefits of Work.
Then in 2013, Monash University (Melbourne) published a world-first study investigating the relationship between GPs and the Return to Work Process including their patient, the insurance agent and the employer.
They found that 96% of claims start in the GP’s office.
They have proposed that the GP is the most important person in the process.
Did you know?
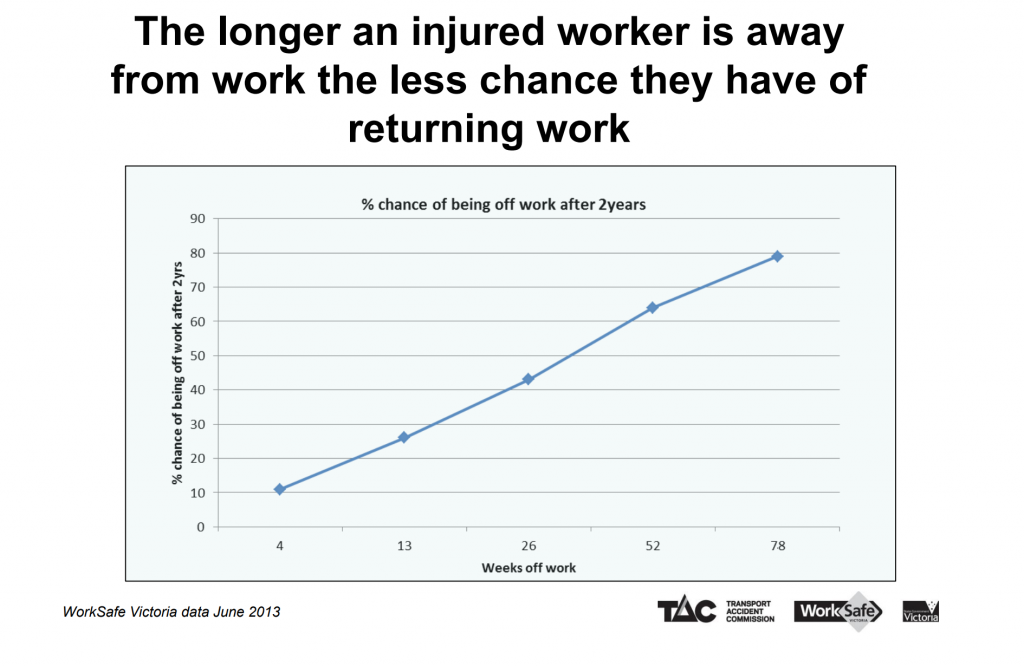
Not only does an early RTW mean greater success in returning to work, it also prevents further insult – such as the development of secondary conditions including psychological conditions, chronic pain and deconditioning.
Did you know?
Both RTW and health outcomes for patients in the compensation sector are often worse than those not in the compensation sector.
This indicates the influence of negative compensation on recovery! While it provides acute financial support and access to treatment and conditioning support, the associated unhelpful beliefs and poor engagement with the RTW process can have serious and negative consequences.
The Health Benefits of Work
Covid19 has highlighted the impact of unemployment. But we knew this before Covid19.
It is well established that working:
- Promotes social cohesion
- Supports a sense of identity
- Provides financial independence for the worker and their family
- Encourages a sense of community
- Can benefit mental health
Conversely, there is a strong positive association between unemployment and increased rates of overall mortality from cardiovascular disease, respiratory disease, mental health disorders, suicide.
Fortunately,
“Work can be therapeutic and can reverse the adverse health effects of unemployment (1)”
As health professionals, we have the responsibility to support people Back To Work.
The Challenge for GPs
Often GPs may feel in the dark, only having information from their patient. This information is, of course, essential! However, injuries are not always straightforward. On top of the obvious physical components, there are the intricacies of the bio-psycho-social influences.
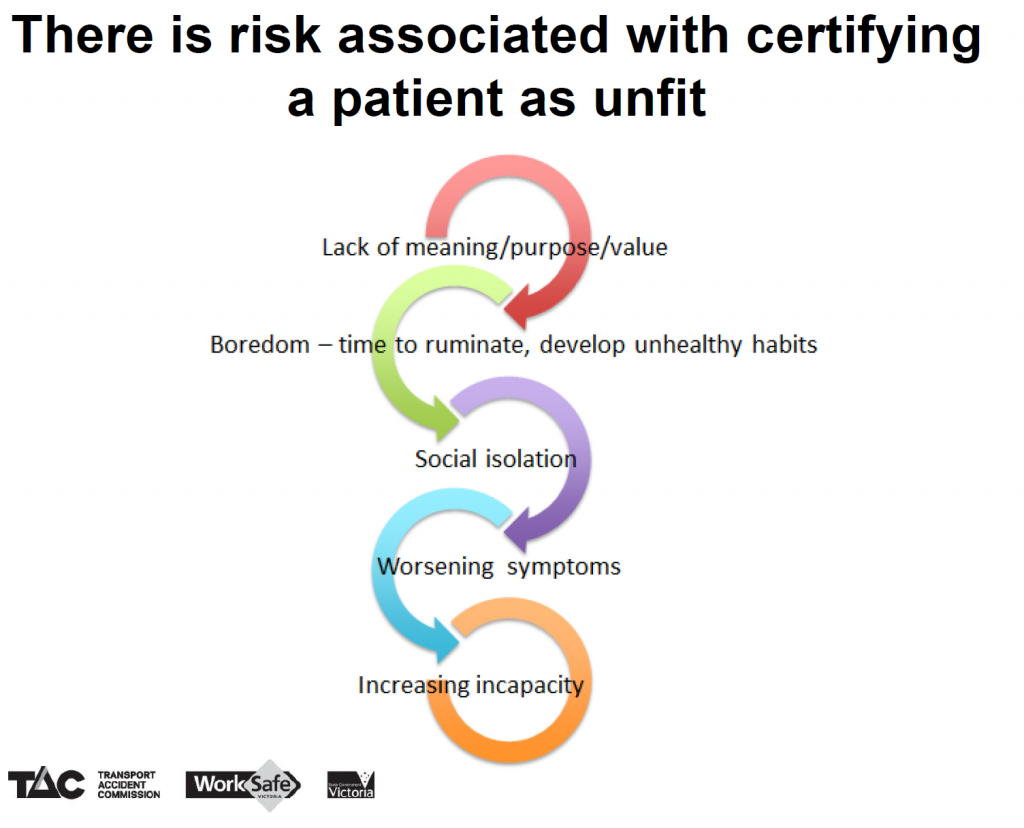
When there is compensation, there are even more layers. It can be easy for the patient to fall into a trap of disempowerment, a focus on disability, and unfortunately iniquitous feelings around the situation.
The GP is expected to make the call on work capacity without having the chance to physically assess the patient in the context of their workplace and physical duties.
With GPs, first and foremost being advocates for the patient, it can be all too easy to become “patient-led,” forgetting the benefits of RTW in the absence of knowledge regarding the whole picture.
We need to foster self-management, patient-responsibility and empowerment.
It’s a tough gig, and we know you’re busy. So we want to help.
What you can do as a GP
“Work is an important part of rehabilitation; Work is a therapeutic intervention” (2)
- Support and encourage a RTW in any capacity
Dr Beres Wenck (Queensland GP with more than 35 years’ experience), believes that “it is important GPs advocate that their patients do some lighter work in the meantime and have an idea of what their job is and how we can try to get them back to work as soon as they are able to do so.” (1)
- Liaise with the other health professionals helping out on the case.
Request reports, if you haven’t already been included. Be open to Case Conferences. Ask questions. Provide recommendations.
“Collaboration results in better outcomes” (2)
Other health professionals, such as Occupational Therapists, Rehab Consultants and Exercise Physiologists, have the information that you need. They are speaking to the employer, they have seen the workplace and the requirements, they have assessed functional capacity and they have an evidence-based, individualised plan to help the patient back to work. But they need your approval.
- When considering the Certificate of Capacity, try to focus on what they can do, rather than what they “can’t” do.
For example, instead of saying “No bending,” you can say “Perform infrequent Bbending as tolerated”
The body was made to move, and fear around movement can be hugely detrimental to a patient’s recovery. By focusing on their abilities instead of their disabilities, you help the patient take a more proactive approach to their recovery. Unfortunately if they are “certified” as “can’t bend” many are too scared to try during treatment, and if they can’t try in a safe supervised environment, how can they ever improve this movement, and get back to a normal life?
“Waiting for recovery, delays recovery” (2)
The Role of an Exercise Physiologist
Exercise Physiologists are the experts in assessing and improving functional fitness, exercise, movement and behaviour change – including providing the strategies for self-management.
Functional fitness is the fitness (strength, endurance, and movement quality) to perform work and life tasks. The lifestyle and exercise program is individualised to your patient depending on your patient’s life, work, injury history, exercise history, comorbidities, beliefs and goals.
We work closely with other health providers and where there are deficits between their work requirements and their current physical capacity, we work to address these. This may include job-specific exercises, manual handling training or liaising with the OT to support the amazing role that they play in the patients recovery.
We focus on function and ability. We focus on empowering the individual. We, and your patient, need you on our side.
“Good outcomes are more likely when individuals understand the health benefits of work, and are empowered to take responsibility for their own situation” (1)
Let us help you and help your patient.
- Brad Domek, Director and NSW Team Leader (brad@specialisedhealth.com.au)
- James Danos, VIC / SA Team Leader (james@specialisedhealth.com.au)
- Lauren Teitzel, QLD Team Leader (lauren@specialisedhealth.com.au)
References & Resources
- Getting back to work, https://www.racgp.org.au/download/Documents/Good%20Practice/2014/June/201406GP_returntowork.pdf
- How to help your patients with work related psychological injury (presentation), Dr Barresi (GP), Dr Cotton (Clinical Psychologist), Dr Fleman (Consultant Psychiatrist) https://www.racgp.org.au/download/Documents/VicFaculty/worksafe.pdf
- Australian and New Zealand Consensus Statement on the Health Benefits of Work
Author: Biara Webster, Exercise Physiologist



