First published April 7 2020
What’s the difference and when you should choose an EP
Rehab processes, especially in the world of Occupational Rehabilitation, almost always involve a multidisciplinary team. Physios, Exercise Physiologists, Vocational Consultants, Occupational Therapists and Psychologists (just to name a few!).
Most of these disciplines are very clear in their delineation and their specialisation there is often confusion between Exercise Physiology and Physiotherapy. One of the most common questions I’ve had in the Compensation Space, from Claims Managers, is
“When should a claimant move from Physiotherapy into Exercise Physiology?”
Physios do an amazing job and they’re essential to the recovery process. But they’re not the only part of the process.
Because there are some similarities and close crossover at the time of progression, it’s not uncommon to be confused.
So, let’s go through the ideal timeline and where both providers fit in.
Working together to optimise recovery
Too often, EPs are forgotten or remembered too late.
A switched-on Physiotherapist, recognises when active rehab, i.e. exercise, needs to take precedence over passive treatment i.e. hands-on.
Exercise Physiologists specialise in prescribing functional exercise, and broader lifestyle modifications. This is particularly important in the rehabilitation process, where barriers can (and often do!) present. Having a professional who is trained in clinical exercise prescription means that any deviations from the plan, both positive and negative, can be quickly addressed.
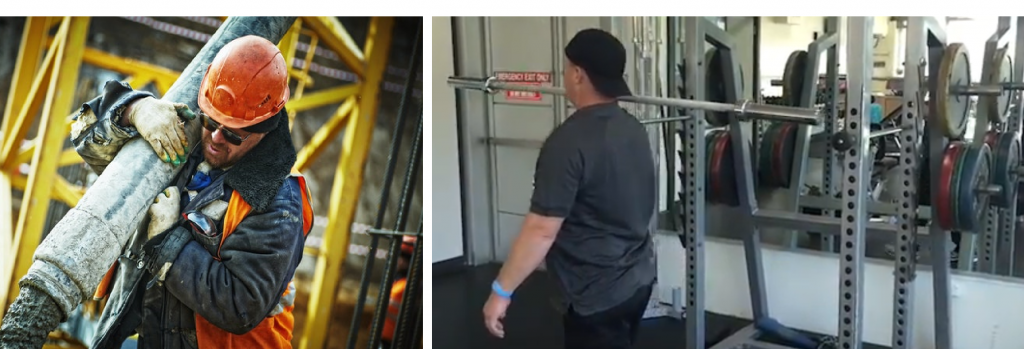
Because our scope and role is primarily in late-stage rehab (12+ weeks), our focus is on exercise prescription to optimise for whole-body functional improvements. In the return to work and life setting, we call this ‘Functional Capacity’ – i.e. the ability to do everyday activities, such as walking, housework, and physical tasks required for work.
This moves the focus away from injury and disability to recovery and ability. It’s about not just getting them back up to 100%, but bringing them to 110%, 120% or beyond.
So, Let’s Put The Timeline Into A Treatment Perspective
A research review, by Costa et al, 2012 found that most acute lower back pain is recovered by 12 weeks. It’s a similar timeline for whiplash too according to the WAD Guidelines issued by SIRA in 2014 – in fact, it’s the expected prognosis for most injuries and surgeries.
In the case of acute injury rehabilitation, physios are your go-to, and Exercise Physiologists are the perfect partner to assist in executing and managing the exercise program set by the physio.
But when it comes to the tricky conditions that persist, Exercise Physiology takes center stage.
Any injury or illness which continues to present after 12 weeks, and is now deemed a “chronic” condition, is now firmly in the specialty area of an EP.
The ideal timeline should look something like this:
Physio: Weeks 0-12
Generally speaking, physiotherapists will diagnose and manage acute conditions through manual therapy (massage, manipulation, needling etc). The earlier they’re involved, the better.
As soon as possible, they should be providing injury specific exercises to improve mobility and minimise strength and function loss, increasing when appropriate.
Using the Whiplash guidelines as an example, they state that at the 6-week mark there should be evidence of improvement, at which stage passive treatment should decrease, with an increase in active treatment (exercise). As treatment transitions from passive to active, it should be monitored closely to ensure that the client is making improvements in their capacity.
Exercise Physiologists: 12+ weeks
Exercises Physiologists work in the management and prevention of chronic conditions – it is our specialty!
This means that for conditions that persist (or plateau) beyond the 3 month mark, referral to an Exercise Physiologist is the best practise.
When To Refer To EP
There are a few things you can consider other than just weeks. Weeks after all, aren’t very individualised. These are some clear markers that your claimant should be seeing an EP:
From a clinical point of view:
-
It is 12, or more, weeks post injury
-
They have reached 90% of functional range of motion – This basically means they can reach 90% of what they need to be able to do to function. (For example, imagine you’re hanging the washing on the line, your hands aren’t directly above your head. To reach the line is functional motion, to bring your hands directly above your head is full range).
-
Their strength on the affected side is 80% of the unaffected side
-
To be able to return to their previous function, they need cardiovascular training or whole-body conditioning
-
They are exhibiting mood symptoms (exercise is an essential part of mental health) (also consider psychology!)
From a Return to Work perspective you should consider engaging an EP when:
-
There is a gap between their current function and the function required in their work role
-
There are no suitable duties available and therefore “real world” conditioning is not able to be performed
-
There are specific milestones to reach to enable progression through a RTW Plan.
-
Clear functional information is required to enable discussions and planning with General Practitioners, Occupational Physicians and other industry professionals
When you work with us
Specialised Health’s Exercise Physiologists prioritise communication, with detailed reports and regular email updates to all parties involved. We are also no stranger to teleconferencing! Our international company has been using it for weekly team meetings and in-services, as well as telehealth services for the last 8 years.
If you’d like to know more about Exercise Physiology and what it can do for you or your customers please feel free to reach out:
Brad Domek, Director and NSW Team Leader (brad@specialisedhealth.com.au)
James Danos, VIC / SA Team Leader (james@specialisedhealth.com.au)
Lauren Teitzel, QLD Team Leader (lauren@specialisedhealth.com.au)