
It’s nearing the end of Movember and some men might be looking forward to shaving their moustache, or maybe they’ve become attached to it!
Either way, we want to help you understand what it’s all about.
It’s about Men’s health.
Why is there a whole month dedicated to Men’s Health? Here’s why:
- Men live on average 4 years less than women.
- Each hour 4 men die from potentially preventable conditions
- The suicide rate is 3 times higher for men
- Men are twice as likely to get skin cancer and 3 times more likely to die from melanoma
So, check in with your friends, brothers, fathers, grandfathers, uncles, cousins and if you’re a man – check in with yourself!
With 1 in 8 men being diagnosed with prostate cancer by the time they’re 85, for today’s article we’re going to unpack Prostate Cancer a little bit.
It is the second most common cancer diagnosed in men in Australia, after lung cancer, second most diagnosed in the country (after skin cancer) and the 3rd most common cancer related death after lung and bowel cancers.
What is it?
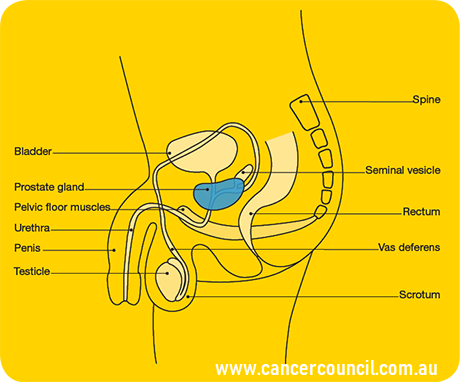
Prostate cancer is an abnormal growth of cells in the prostate gland which form a malignant tumour.
According to the Cancer Council, factors that cause Prostate cancer are: age, particularly over 50 (although younger men are not fully exempt), family history of prostate, breast or ovarian cancer, a diet high in fat and low in fruit and vegetables and a history of high testosterone.
Early Detection
Symptoms of Prostate Cancer include frequent urination (especially at night), pain during urination, a weak stream, blood in the urine or semen, pain in the back or pelvis.
At this stage the only early diagnostic measure available is the blood test PSA (prostate specific antigen), however this does not constitute as diagnosis itself. Some men with prostate cancer actually have normal PSA levels and 1 in 3 men with elevated PSA have the cancer. The test also needs to be repeated over time to measure changes. You can talk to your GP about ordering a test if you’re worried.
Diagnosis
A true diagnosis can be provided through a biopsy, possibly in conjunction with an MRI, CT or bone scan.
Treatment Options
There are a variety of treatment protocols. Surgery removes the prostate gland and surrounding tissues. Radiotherapy can be external or internal. Androgen Suppression Therapy is another option. It is a type of hormone therapy, pharmacologically inducing suppression of testosterone production or the binding sites. It works because prostate cancer is responsive to testosterone.

Prostate Cancer & Exercise
Prevention
A physically active lifestyle provides some protective points against Prostate Cancer by strengthening the immune system. Being physically fit and active is also effective at decreasing complications and death after prostate cancer diagnosis, but assisting in body weight management as well as muscle conservation.
During & After Cancer
Exercise has been shown to enhance many cancer treatments by improving treatment delivery to the cancer cells.
Exercise both during and after cancer is important to assist in the management of side effects. Specific to Prostate cancer, with the hormone changes from Androgen Suppression Therapy, men go through numerous physiological changes including decreased muscle, increased fat and decreased bone strength, which exercise can, at least, partially negate.
Prostate surgery can also result in urinary incontinence and pelvic floor exercises can assist this.
Similar to other types of cancer, exercise can assist managing cancer related fatigue, mood, cognitive function, appetite (which often decreases) as well as increase the chance of survival and decrease the risk of occurrence.
Exercise Tips
- Aim for at least 30 minutes of moderate aerobic activity 5 days per week, such as walking, jogging or swimming and 2-3 strength training sessions per week
- Avoid cycling due to the pressure on the prostate (only with prostate cancer, moderate cycling is OK without cancer)
- Ease your way into exercise, especially if you’re new to it. Your body is already under stress from both the cancer and the treatment.
- Exercise at a comfortable temperature
- Warm up and cool down
- Drink plenty of water
- Consider joining a class (for social health!)
- Enjoy!

Biara Webster
Exercise Physiologist and Writer/Content Manager

Each month we will pick a question to Q&A.
Send your questions to brad@specialisedhealth.com.au or biara@specialisedhealth.com.au
Or contact us through the below social media outlets!
Resources
http://www.49.com.au/assets/Resources/F49-Mens-Health-ToolKit.pdf
http://prostatecancer.org.au/PCI/Exercise_%26_Diet.html
https://www.cancercouncil.com.au/prostate-cancer/
More references
Cormie, P., et al., (2018), Clinical Oncology Society of Australia position statement on exercise in cancer care, The Medical Journal of Australia , https://doi.org/10.5694/mja18.00199
Dickerman, B. A.et al., (2017). Weight change, obesity and risk of prostate cancer progression among men with clinically localized prostate cancer. International journal of cancer, 141(5), 933–944. doi:10.1002/ijc.30803
Cormie, P., et al (2015), A Qualitative Exploration of the Experience of Men With Prostate Cancer Involved in Supervised Exercise Programs, Oncology Nursing Forum






